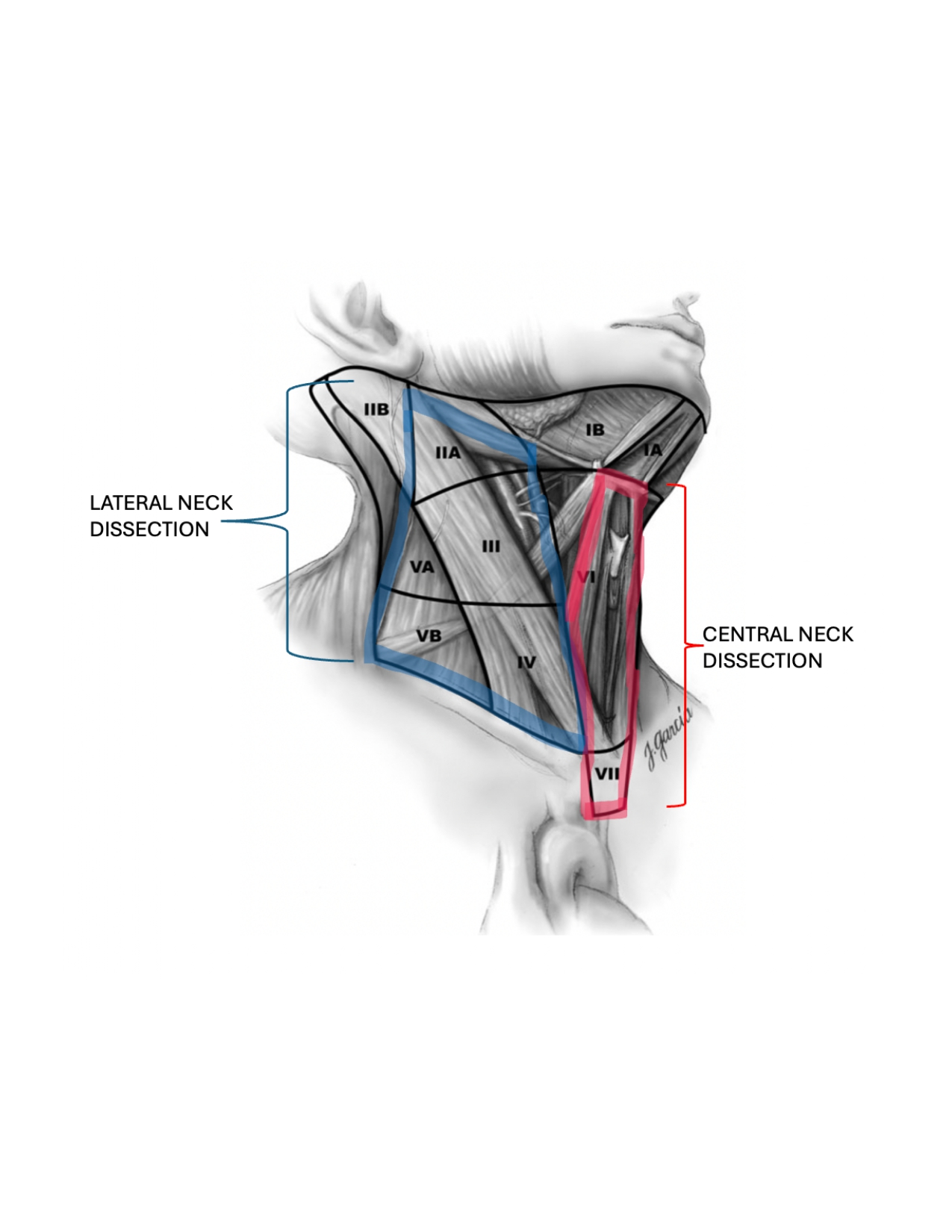
If there is objective evidence of the cancer having spread to the lymph nodes in the neck prior to surgery, or incidentally discovered during surgery, the entire thyroid needs to be removed (total thyroidectomy) and all lymph nodes in that compartment (central neck dissection and/or lateral neck dissection) need to be removed.
- If the cancer has spread to lymph nodes in the lateral neck compartment, it is assumed that it has already spread to the lymph nodes in the central neck compartment first (even if not obvious on imaging prior to surgery).
- Both central and lateral neck dissections should be performed.
- Prophylactic central neck dissections (without objective evidence of cancer spreading to a lymph node) are not indicated unless extrathyroidal extension (cancer invading through the capsule of the thyroid into nearby structures) is noted on imaging before surgery or appreciated clinically during the surgery.
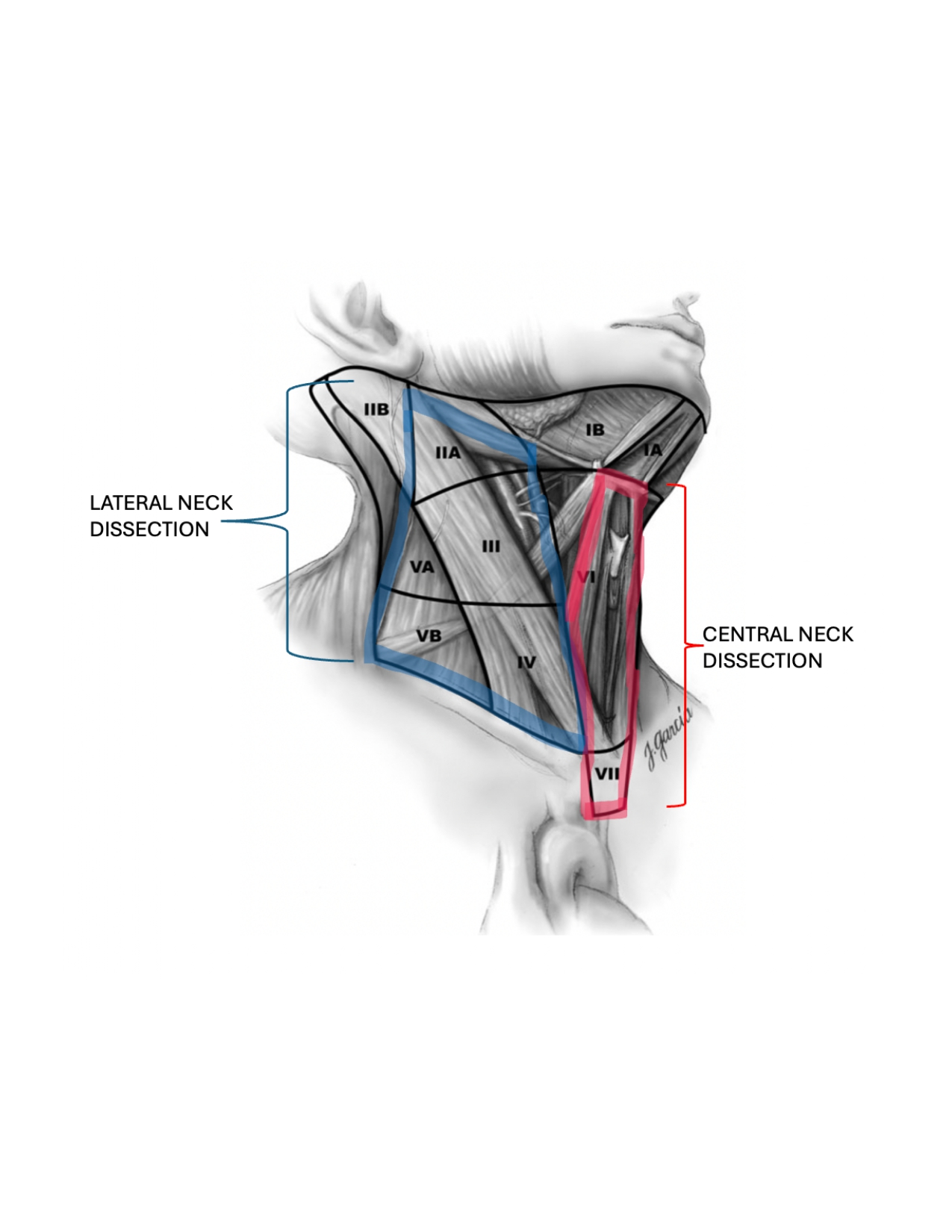
Image Source: Mary Ann Liebert, Inc.
If the cancer has not objectively spread to the lymph nodes in the neck, American Thyroid Association (ATA) Guidelines state survival rates are similar for hemithyroidectomy (removing only one half of the thyroid) and total thyroidectomy (removing the entire thyroid) if the cancer is < 4.0 cm, no obvious extrathyroidal extension (invasion into the nearby muscles, trachea, or esophagus), and no high suspicion nodules in the other thyroid lobe.
- A cancerous thyroid nodule should NOT be ‘carved out’ of a thyroid gland in order to preserve thyroid function.
- This increases the risk of leaving cancer behind, increases the risk of injuring the recurrent laryngeal nerve causing temporary or permanent voice changes, and would make potential revision surgery in the future far more difficult.
- For this reason, recommendations from the ATA are to remove at least the entire lobe of the thyroid where the cancer is present.
- When removing half of the thyroid, ~70% of the time the remaining half makes enough thyroid hormone to prevent hypothyroidism.
- 30% of the time the remaining half does not make enough thyroid hormone and you must be on a once daily thyroid hormone medication for the rest of your life to prevent hypothyroidism.
- This risk is increased the higher the pre-surgery TSH levels are and the smaller the size is of the remaining thyroid lobe.
- Thyroid hormone levels in the blood are measured 6 weeks following surgery to check for this.
- It takes this long for all the old thyroid hormone to filter out of the blood and to get an accurate measurement of how much hormone the remaining half of the thyroid is making.
- It is relatively rare to develop signs of hypothyroidism during this 6-week period before obtaining blood work. If you do, consider contacting your doctor for earlier labs.
- If only half of the thyroid is removed, but high-risk features are discovered on the pathology report or 6-week post-operative thyroglobulin (tumor marker) levels are elevated suggesting residual cancer, the remaining half of the thyroid should be removed to maximize survival chances.
- This second surgery should be performed within 2 weeks of the original surgery before too much scar tissue and inflammation forms complicating the surgery and increasing the associated risks.
- Otherwise, the surgery should be delayed 3 months, when the scar tissue and inflammation has sufficiently resolved.
- Waiting 3 months for treatment of WDTC’s does not significantly increase the risk of further growth or spread of the cancer, or increase the risk of dying from the cancer.
Sometimes unexpected invasion of the cancer into nearby structures or spread of the cancer to the lymph nodes is discovered during the surgery despite best efforts to rule this out prior to surgery.
- In these scenarios, your surgeon will act in your best interest and perform the surgery that will give you the best chance of a cure – total thyroidectomy with central neck dissection.
For all types of thyroid cancer, surgical outcomes / cure rates are the highest and complication rates are the lowest when surgery is performed by a high-volume surgeon (> 50 thyroidectomy surgeries per year).
To read more about Thyroid and Neck Dissection surgeries including what to expect, as well as details regarding recovery and risks: